Asteroid Medical Billing is a leading, Credentialing and Medical Billing Company
Asteroid medical billing offers end to end complete RCM solutions and focused on providing customized services with good quality to the professionals in the healthcare industry.
After 16+ years of experience in the RCM medical billing field
We started this company, with six agents as a small office and past 3 years we have grown substantially to serve numerous clients who help business through referrals and other marketing strategies. We have grown from a humble beginning and we serve and give solutions to the end to end revenue cycle management.
Our goal is to Simplify your administrative burden and set a goal to maximum your reimbursement
Expertise
Our team has vast experience in medical billing.
Efficiency
We streamline the process to ease your administrative workload.
Communication
We ensure transparent and consistent communication so that you are always kept informed.
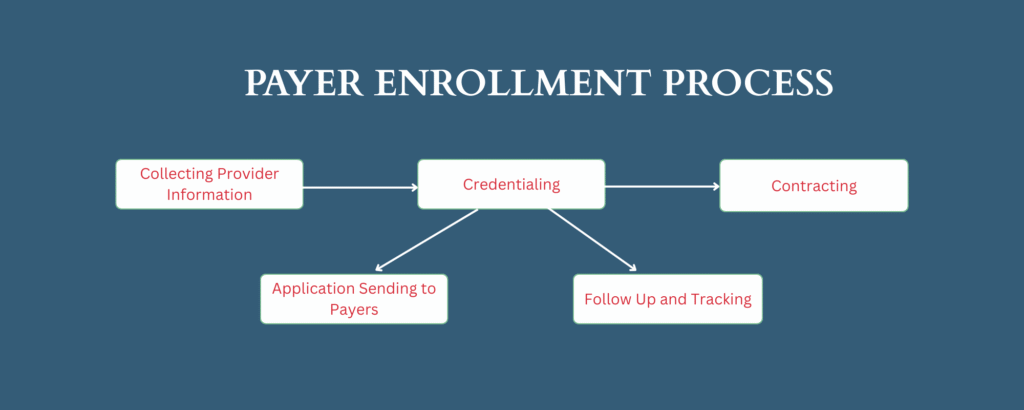
We do various clearing house settings and payment enrollment process like EDI, ERA & ACH/EFT
We do credentialing for Laboratory service to all state and island.
Asteroid Medical Billing offer below mentioned list of services
ELIGIBILITY
FOR ACCURACY BILLING
AUTHORIZATION
PRE AUTH & RETRO AUTH
CODING
CERTIFIED CODERS
DEMO & CHARGE ENTRY
QUALITY CHECK & CLAIMS TRANSMISSION
AR RECOVERY
CLAIMS FOLLOW UP
PAYMENT POSTING
POSTING & SECONDARY CLAIMS FILING
DENIAL MANAGEMENT
RESOLUTION FOR DENIALS
AR CALLING
FOLLOWUP ON UNPAID CLAIMS
PATIENT BILLING
OUT OF POCKET EXPENSES
COLLECTION & REVENUE ANALYSIS
WEEKLY AND MONTHLY WISE
REPORTS
CUSTOMIZED REPORTS PER CLIENT NEED
Our mission is to revolutionize the healthcare industry by providing innovative solutions that empower healthcare practices to thrive.
We understand the challenges as we faced those challenges previously and resolved them through our experience in billing, coding, denial management and in practice collection.
Our team delivers cutting-edge technology to optimize revenue cycles and ensure best financial reimbursement outcomes for our clients.
We operate with the utmost care of integrity and we ensure compliance with healthcare industry regulations and maintain the confidential of patient data.
Our excellence drives our service to stay ahead with the industry trends and best practice.
Adopting the latest technologies and developing creative solutions which keeps to drive your practice forward.
- Availibility
- Responsiveness
- Reliable
- Support


Asteroid Medical Billing have experience in handling nearly 30 plus specialties. Few major specialties listed below that we take pride in servicing clients are
- Allergy & Immunology
- Anesthesiology
- Behavioral and Mental Health
- Cardiology
- Cardiovascular Disease
- Chronic care management (CCM)
- Chiropractic
- Critical care
- Family Medicine
- Gastroenterology
- Geriatric
- General Medicine
- Hospital Billing
- Infectious Disease
- Internal Medicine
- Nephrology
- Neurology
- Nursing Practitioner
- Obstetric & Gynecology
- Oncology
- Orthopedics Surgery
- Pain Management
- Pathology
- Physical Therapy
- Pediatrics
- Podiatry
- Psychiatry & Mental Health
- Psychiatry & Neurology
- Pulmonary Disease
- Rheumatology
- Radiology
- Sleep Medicine
- Surgery
- Transitional Care Management (TCM)
- Tele Visit
- Urgent Care
- Urology
- Wound Care
Our streamlined workflow ensures efficiency and accuracy from patient registration to payment collection. Each step is meticulously managed to optimize billing processes and improve overall revenue cycle performance.

1. Patient Registration – Capture and verify patient details to ensure accurate recordkeeping.
2. Eligibility – Confirm insurance coverage and benefits before providing services.
3. Authorization – Obtain necessary pre-authorizations for coverage of specific services.
4. Coding – Assign accurate ICD-10 and CPT codes for diagnoses and procedures.
5. Demo & Charge Entry – Input patient demographics and service charges into the billing system.
6. Payment Posting – Record and apply payments from insurance and patients to accounts.
7. AR Calling & Follow-Up – Follow up with insurance companies and patients on outstanding balances.
8. Patient Billing – Generate and send billing statements to patients and manage payment plans.

We harness state-of-the-art technology to transform medical billing into a seamless, efficient process. Our cutting-edge software solutions and advanced automation tools are designed to tackle the complexities of healthcare billing with precision and speed.
We Are Here To Help With Your queries !
How is accuracy ensured in medical billing?
Accuracy in medical billing is achieved through the use of advanced technology that automates data entry and processing. Real-time validation checks and comprehensive coding tools are employed to ensure that all billing information is precise and compliant with current regulations, minimizing human error.
What measures are taken to reduce claim denials?
To reduce claim denials, sophisticated software is used to identify and correct potential issues before claims are submitted. This includes thorough audits of coding and documentation to prevent errors and omissions that could lead to rejections. These proactive steps increase the likelihood of claim approval and expedite reimbursement.
How is the billing process streamlined?
The billing process is streamlined through integrated solutions that automate manual tasks such as claim creation, submission, and payment tracking. This automation reduces the need for manual intervention, shortens turnaround times, and improves overall efficiency in billing operations.
How is regulatory compliance maintained?
Regulatory compliance is maintained by utilizing technology that is regularly updated to reflect the latest industry regulations and coding standards. Continuous updates ensure that billing practices adhere to current guidelines, helping to prevent errors and maintain accuracy.
What benefits does data analytics provide for billing management?
Data analytics offers valuable insights into billing operations, including performance metrics, payment trends, and claim status. Analyzing this data helps identify areas for improvement, optimize revenue cycles, and make informed decisions to enhance financial performance and operational efficiency.
